Navigating the complexities of prostate cancer, many grapple with concerns like “how does prostate cancer cause death?” and ponder over the chances of prostate cancer returning after surgery. Individuals diagnosed with localized or locally advanced prostate cancer generally have a more favorable survival outlook compared to those with metastatic disease. Staging is vital as it determines the extent of the tumor’s spread, often to bones or other parts of the body. Some may even wonder what is the longest someone has lived with stage 4 prostate cancer. As the cancer advances, survivors may face challenges like pain from nerve involvement, weakened bones, or digestive complications including loss of appetite and diarrhea.
The Biology Behind Prostate Cancer Progression
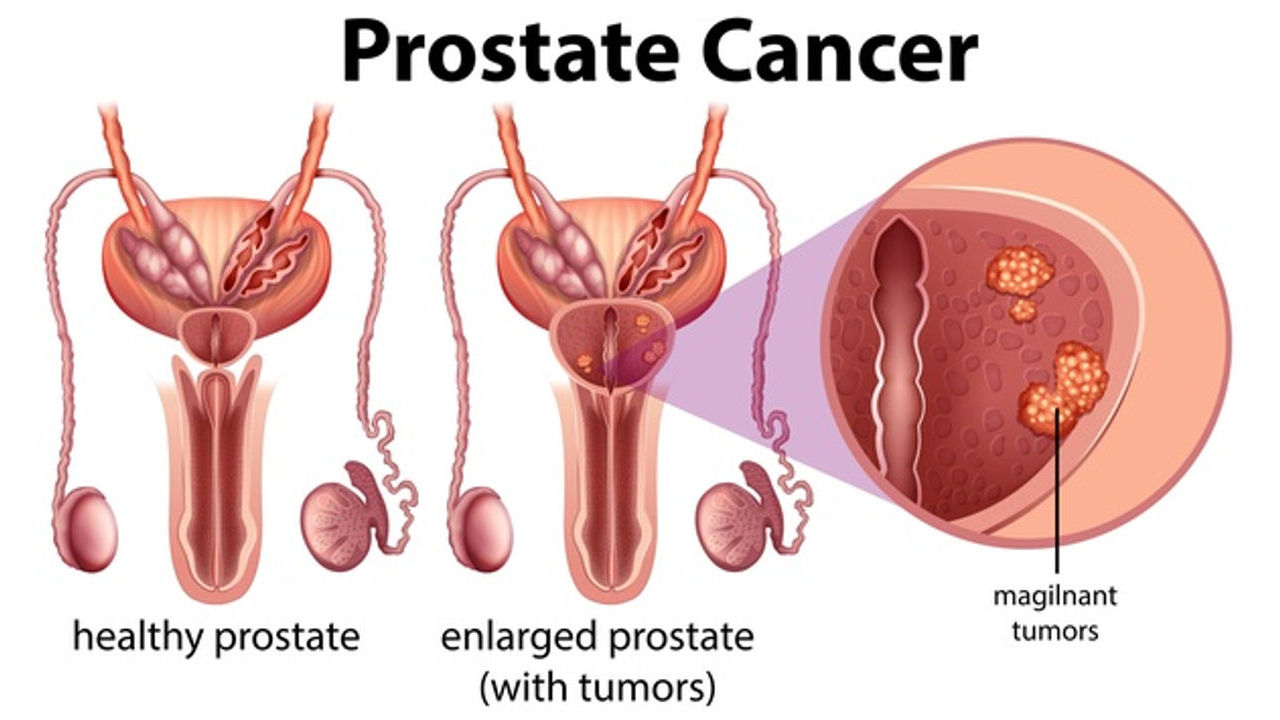
Cancer occurs when cells in the body start growing out of control and no longer die when they should. Instead, these rogue cells continue dividing and creating more cancerous cells which then spread throughout other parts of the body via metastasis.
Early diagnosis through screening for high levels of PSA offers men the best chance of curing their disease; however, due to its progressive nature some men who develop it will eventually succumb to its effects and die as a result.
Immunotherapy and focal therapies offer additional ways of treating prostate cancer beyond surgery, radiation and hormone therapy. These novel approaches target genetic mutations that drive its progression while simultaneously eliminating resistant cells that have proven evading conventional treatments.
Symptoms of Advanced Prostate Cancer
Even with PSA screening, most deaths from prostate cancer happen after its spread or metastasis to other parts of the body – specifically when advanced stage disease has spread beyond being contained within just the prostate gland. This disease tends to metastasize more readily when no longer restricted solely by this physical boundary.
Men in stage 3 may notice weak urine flow or pain when they urinate (dysuria). At later stages, there may be an urgency to urinate which leads to blood in their urine (hematuria) and difficulty passing urine (urinary incontinence).
As cancer spreads, it can encroach upon nerves and lead to discomfort in the groin or back area. Furthermore, cancerous tumors put pressure on spinal cord and disrupt its normal operation, leading to backache symptoms.
Advanced prostate cancer cannot be cured, but treatments can slow its progress and keep it under control for years. Doctors use statistics to estimate how long a person might survive post diagnosis of cancer and treatment start; these rates are known as survival rates; every individual will have different chances of survival so be sure to discuss your chances with your healthcare provider.
Metastasis: Prostate Cancer’s Deadly Turn
Cancer often spreads beyond its initial source in prostate gland. Cancer cells acquire mutations that switch on genes that promote growth and replication while disabling those which would normally slow cell division or lead to their eventual demise, eventually multiplying exponentially and crowding out healthy ones.
At some point, prostate cancer cells break off and travel through blood vessels to other organs. Sometimes this causes symptoms or may only be diagnosed once advanced stages have been reached.
Research using SEER data found in 2021 that men with metastatic prostate cancer had a 34% to 19% increased risk of dying from noncancer causes than age-matched males without it, according to a JAMA Network Open study. Death typically results from heart disease, stroke or chronic obstructive pulmonary disorder (COPD).
Men with prostate cancer that has spread can qualify for palliative care to alleviate their symptoms and enhance quality of life. Medication to control symptoms and enhance quality of life as well as treatments like immunotherapy and focal therapy to target and destroy cancer cells may all play an essential part of palliative care treatment plans.
The Role of PSA Levels in Monitoring and Detection
A PSA test measures the levels of prostate-specific antigen (PSA), a protein produced in your prostate gland, in your blood. An elevated PSA level may signal an increased risk for prostate cancer.
When a man has an elevated PSA level, their doctor will closely monitor it to see if it increases quickly or not. A sudden surge is known as “PSA velocity” and could indicate they have an aggressive tumor that spreads more quickly than usual.
Doctors will also keep an eye on the percentage of PSA that remains free and unbound to other proteins in your blood, known as free to total PSA ratio (FRPSA). A lower FRPSA could indicate more aggressive tumors with greater potential to spread quickly.
Additionally, your doctor may conduct a digital rectal exam (DRE) to detect signs of tumor development such as hard bowel movements or increased ejaculation that could potentially increase PSA levels. They’ll consider these factors and your age before suggesting a screening schedule for serum PSA levels.
Many men with indolent prostate cancer do not require treatment since their tumors grow slowly and never reach life-threatening stages. On the other hand, some men diagnosed with aggressive forms will eventually succumb to it even if detected at an earlier stage than expected.
Importance of Early Diagnosis and Treatment
Men may experience symptoms that indicate prostate cancer, including blood in their urine, difficulty or pain while urinating and difficulty passing urine. While these signs could also occur with benign prostatic hyperplasia (enlarged prostate), doctors usually use imaging tests such as an MRI or transrectal ultrasound followed by biopsy to diagnose. To do this accurately and quickly, samples from prostate tissue may then be examined under a microscope in order to detect spread or slow growth – known as indolent prostate cancer.
Cancerous conditions often progress to later stages, which are measured by how far their cancer has spread from its original site of origin. Stage 1 indicates that cancer has not spread beyond the prostate gland itself; Stage 2 can be subdivided into substages such as 2A and 2B to indicate when cancer has reached nearby tissues without spreading beyond. Finally, Stage 3 includes substages like 3A and 3B that indicate when lymph nodes or distant sites in the body have been infiltrated by cancer cells.
Age can play a significant role in an individual’s risk for prostate cancer, with two-thirds of those who die from it being over 75. Men of African descent are twice as likely to develop prostate cancer compared to other races, and it tends to be advanced at diagnosis.
Contemporary Treatment Options and Their Impact
As early screening and treatment advances have increased survival rates for most men with prostate cancer over the last 50 years, their survival rates have more than tripled. Unfortunately, advanced prostate cancer remains fatal at high rates; its symptoms including increased pain as well as other health problems that are difficult to treat can still claim lives in its late stages.
Many men with low-risk prostate cancer may be able to sidestep surgery and radiation therapy by having their doctor use active surveillance. This involves regular screenings and biopsies to keep an eye on cancer growth as well as for any signs of spread; should this happen, the doctor can then implement treatments either to stop its further spread or attempt a cure.
Radiation therapy and brachytherapy are also viable localized treatment options, using radioactive seeds inserted directly into the prostate gland to deliver radiation directly to tumors. Brachytherapy seeds may remain there either temporarily (high-dose rate) or for longer depending on your circumstances.
Preventive Measures to Reduce Risks
Like other health conditions, prostate cancer has both risk factors we can control and ones we cannot. Diet and lifestyle modifications may help lower our risks; however, factors like age and race cannot always be altered directly.
Reduce our cancer risk by eating less red and processed meat, opting instead for leaner cuts of beef, fish or plant-based proteins such as beans. Also include in your diet more cruciferous vegetables like broccoli and cauliflower which contain sulforaphane which has been found to prevent some forms of cancer.
Consuming more leafy greens such as kale and Swiss chard may help lower cancer risks. These vegetables contain Vitamin A, which has been proven to prevent tumor development. Also incorporating foods rich in antioxidants like tomatoes and berries may further lower our risks.
One effective prevention measure is exercise regularly and maintaining a healthy weight. Studies have linked obesity with higher prostate cancer risks; additionaly, we can lower our stress levels through meditation or other forms of relaxation techniques.